SF3B1 mutations are the most frequent spliceosomal alterations across cancers, yet no successful therapy exists to target this pathway. Previous findings from a phase 2 clinical trial of the XPO1 inhibitor selinexor in patients with high-risk myelodysplastic syndrome (MDS) relapsed or refractory to hypomethylating agents (HMA) revealed increased activity in patients with SF3B1 mutations. XPO1 (Exportin-1) is responsible for the nuclear export of over 200 proteins, but also plays a role in the transport of multiple RNA species, including small nuclear RNAs (snRNAs), ribosomal RNAs (rRNAs), and select messenger RNAs (mRNAs) out of the nucleus. Given the role of XPO1 in exporting snRNAs, which form the catalytic portion of the spliceosome, we hypothesized that XPO1 inhibition may preferentially affect SF3B1-mutant cells via altered splicing, and that SF3B1-mutant high-risk MDS patients would have a better response to rational targeted drug combinations with next generation XPO1 inhibitors.
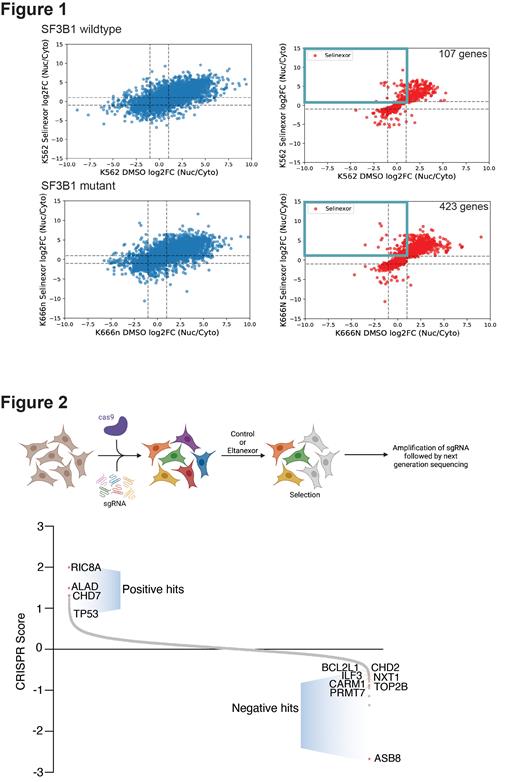
To evaluate the mechanism underlying the preferential sensitivity of SF3B1-mutant cells to XPO1 inhibition, we performed nuclear and cytoplasmic fractionation followed by RNA sequencing (subcellular RNA-seq) before and after XPO1 inhibition in SF3B1 wildtype and SF3B1 K666N mutant cells. Whole transcriptomic analysis of subcellular RNA-seq data revealed increased global retention of RNA transcripts in the nucleus after XPO1 inhibition in the SF3B1 mutant cell line ( Figure 1).
Validation assays using qPCR confirmed nuclear retention of several key transcripts such as Salt Inducible Kinase 1 (SIK1) and Cancer/Testis Antigen Family 45 Member A2 (CT45A2) in SF3B1-mutants (both SF3B1 K666N and K700E). Similarly, we performed subcellular RNA-seq for small RNAs and found snRNAs to be increased in the nucleus after XPO1 inhibition in the SF3B1 mutant cells. We then performed total cellular RNA sequencing to understand the effect of XPO1 inhibition on global RNA expression and RNA splicing. Differential gene expression analysis revealed that XPO1 inhibition had a more pronounced effect on cell cycle in SF3B1 wildtype cells, but differentiation pathways were more significantly affected in SF3B1-mutant cells. Alternative splicing analysis showed increased 3' alternative splicing events in SF3B1 mutant after XPO1 inhibition. These results suggest that the preferential sensitivity of SF3B1 mutant cells to nuclear export inhibition arises through increased nuclear retention of spliceosomal snRNAs and select mRNAs that results in perturbation of differentiation pathways.
Despite the promising efficacy of XPO1 inhibition in SF3B1 mutated MDS, toxicity limits its dose escalation. Combination therapies may allow for greater synergism with lower doses of XPO1 inhibitor. In order to identify novel drug combination targets, we employed whole genome CRISPR screens in two myeloid leukemia cell lines treated with eltanexor, a next generation XPO1 inhibitor with lower toxicity than selinexor ( Figure 2). These analyses identified several novel targets, which we validated by testing for synergy in combination with eltanexor in wildtype and SF3B1-mutant cell lines. Using the Bliss independence model to calculate synergy, we identifed two drugs that greatly synergized with eltanexor specifically in the SF3B1 mutant cell lines: venetoclax (a BCL2 inhibitor), and navitoclax (a BCL2/BCL-XL inhibitor). We further validated these combinations in vivo using competitive transplant assays in Sf3b1 K700E conditional knock-in mice. The combination of eltanexor with venetoclax showed a significant decrease in the Sf3b1-mutant burden in the peripheral blood and bone marrow progenitor compartments, suggesting a preferential sensitivity of the combination for SF3B1 mutation.
In conclusion, by analyzing the effects of XPO1 inhibition on RNA export, our study provides insight on the mechanisms behind the increased efficacy of XPO1 inhibition in SF3B1-mutant MDS/AML. Our findings may also contribute to the development of potentially synergistic therapeutic combinations. In this regard, recent human data have shown that venetoclax can overcome the poor prognosis of spliceosomal mutant AML patients (Senapati et al, Blood 2023); therefore, combining eltanexor with venetoclax could represent a promising SF3B1-specific therapy.
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal